THE PROBLEM
DD affects people in many different ways, some have few or no symptoms and their lifestyle is unaffected. Others are simply too ill to even think about leaving their home. These extremes can be a permanent or temporary situation for many sufferers. Older, retired people with DD sometimes have a different problem. An organiser of outings for an over-60s club said that people with DD could not go on their trips because they dare not go away from a toilet. That was 3 decades ago and not much has changed since then. Some coaches now have on-board toilets but public transport and car journeys also present problems. Apprehension and nervousness before a holiday, meal or outing, even a pleasurable one, sends their guts into overdrive. There is no mention of this problem in medical or self-help books or websites. It is not a topic of conversation even with close relatives and comedian’s jokes do not help.
This is a ‘flight or fight’ reaction of the sympathetic nervous system which empties the bowel and bladder. This is also experienced by actors, singers, sportsmen and women etc. but with performers, when the bowel has emptied and work begins, things can settle down. A bowel with DD which is damaged in structure and nerve control does not always produce a normal reaction. A second factor can be the major movements of the bowels which usually take place on rising/breakfast, so that early morning is a common time for bowel evacuation. A high-fibre diet often recommended for people with DD means that the bowel is relatively full. A combination of these factors can produce quite distressing results and avoiding the trigger situation is a natural reaction
HELPFUL TIPS
When this problem was raised in a former patient support group there were several helpful suggestions based on member’s experience. Giving in to the situation can lead to a downward spiral resulting in becoming housebound and loss of social activities. Looking back, contributors thought they worried far too much and this made the problem worse. Making outings less of an ‘event’ and more frequent can send the spiral upwards. Realising what was happening and knowing the location of toilets often helped. Other tips were…..
- Allow sufficient time for the bowel to be emptied before setting out, once empty it will settle down
- Avoid constipation so that there are less faeces to evacuate
- Have a low fibre diet for a few days beforehand for the same reason
- Get up early for a few days beforehand
- Make appointments for afternoons if possible
CAN DRUGS BE USED TO EASE THE PROBLEM ?
Some sufferers reported short term tranquilisers or herbal remedies had helped. Antidiarrhoea drugs are the most obvious and easily purchased solution, but their use is not clear-cut. The BNF (British National Formulary, an official guide to drug use) says that antimotility drugs (codeine, diphenoxylate, loperamide) are contraindicated for DD because they could exacerbate symptoms. On the other hand, if the problem is called “IBS” rather than “DD” then loperamide can be used to relieve diarrhoea. (An anomaly of dual diagnosis!) Advertising promotes the immediate beneficial effects of loperamide but not that bowel movements can be prevented for several more days. Your doctor or pharmacist should advise on a personal basis whether antidiarrhoeal drugs are suitable.
WHAT DOES THIS TELL US ABOUT DD?
There is another way of looking at this problem. Some apprehension, bustle and early rising are clearly a good laxative which is unrelated to diet, food supplements or fibre levels. Perhaps this observation might be used to good effect. Not defaecating in the morning is a risk factor for constipation in DD patients (1).
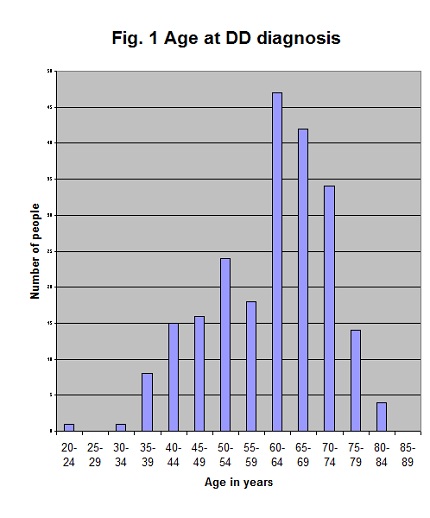
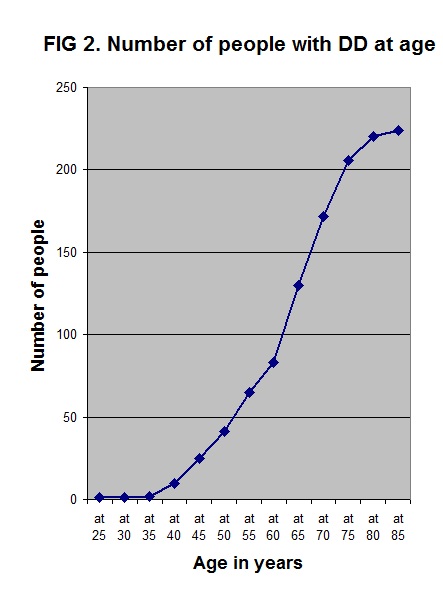
Are retirement and/or no longer going out to work early in the morning behind the housebound problem? This change in lifestyle when age is also slowing down bowel function would tend to produce constipation. Is this the time when symptomless diverticulosis changes to symptomatic diverticular disease and medical help? A support group survey showed that diagnosis of DD occurred at retirement ages (Fig 1). This is the same as in the 1970s in Belfast (2). The diverticula had formed before retirement age. Exactly the same data is presented in Fig. 2 in the cumulative form which is often found in DD research statistics. This gives the impression that DD incidence continues to increase with age rather than that people with DD get older.
Diagnosis as a result of diverticulitis can occur any time when diverticula are present. Reports are increasing of cases quite early in life – in 20s and 30s age groups. This shows that diverticula can be formed at a young age and not neccesarily as a result of a lifetime of low-fibre diet or only related to old age. There may be different time scales for cause, formation of diverticula, infections and functional symptoms of DD.
REFERENCES
(1) Osipenko MF & Bikbulatova EA Colon diverticula: origin, prevalence, clinical maefestations. Ter Arkh 2007, 79, 26. (PMID 17460964)
(2) Parks TG Natural history of diverticular disease of the colon. Clinics in Gastroenterology. 1975, 4, 53.
© Mary Griffiths 2010
NOTE This article appeared in the Journal of the Bladder and Bowel Foundation, Issue no. 5, Summer 2010, and is also available in the professional resources section of their website
Tags: ageing, Diagnosis, Drugs, Statistics, Symptoms